Autoimmune and inflammatory conditions often stretch across months or years, with symptoms that flare, fade, and return unexpectedly. Many people explore supportive options not because they expect a miracle, but because they want steadier control over symptoms and faster healing when inflammation damages tissue.
Hyperbaric oxygen therapy fits this interest thanks to its role in improving tissue oxygenation and helping circulation reach areas that struggle during chronic inflammation.
So the question arises, can HBOT realistically support pain reduction, shorten flare recovery, or improve fatigue? Let’s see what the answer is.
How HBOT Works Inside the Body
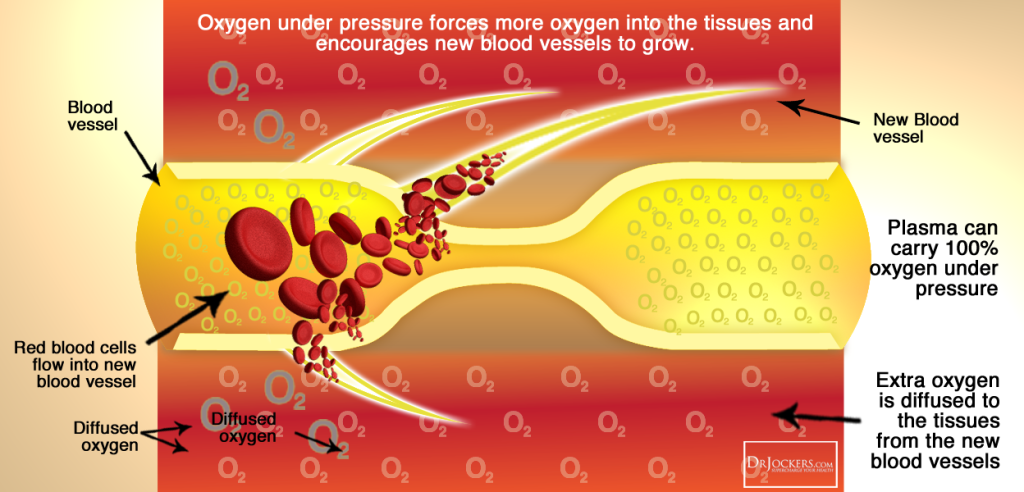
Hyperbaric oxygen therapy increases the pressure around the body, allowing much higher levels of oxygen to dissolve into the bloodstream. This extra oxygen can reach inflamed or poorly perfused tissues more effectively than normal breathing conditions allow.
Below are key mechanisms that matter for autoimmune and inflammatory conditions:
- Higher oxygen levels support tissue repair and collagen formation.
- Improved microcirculation can help areas affected by swelling.
- Oxygen-rich environments may shift inflammatory signaling toward a calmer state.
- Mitochondria work more efficiently when oxygen is abundant, which may help ease fatigue.
These internal shifts happen gradually across multiple sessions, which is why consistency matters more than any single treatment.
Tissue hypoxia means cells are not receiving enough oxygen to function normally. HBOT is designed to correct this imbalance.
Evidence Highlights and What Researchers Have Observed
While research varies by condition, several consistent patterns appear across clinical observations.
Here is a clear summary showing what HBOT has demonstrated in studies so far:
| Research Focus | Observed Effects | Notes |
| Immune regulation | Reduction in inflammatory markers and increased anti-inflammatory activity | Seen in both human and animal studies |
| Tissue repair | Faster healing in inflamed or damaged tissue | Often reported in joint, skin, and soft-tissue conditions |
| Chronic pain | Increased pain threshold and lower muscle tenderness | Especially noted in chronic musculoskeletal inflammation |
| Post-flare recovery | Reduced swelling and quicker functional recovery | Frequently reported by patients undergoing regular sessions |
These findings do not claim HBOT cures autoimmune disease. Instead, they point to biologically meaningful support that strengthens the broader treatment plan already in place.
Conditions Where HBOT Is Most Commonly Discussed

Autoimmune and inflammatory disorders share overlapping features, which is why HBOT is studied across different diagnoses. Many of the conditions below involve tissue damage, chronic inflammation, or reduced oxygen supply.
- Rheumatoid arthritis: Joints affected by swelling may respond to improved microcirculation and oxygenation.
- Inflammatory bowel disorders: Intestinal tissue healing is often supported by better oxygen access.
- Psoriasis and chronic skin inflammation: Skin affected by immune-driven irritation may heal more effectively under oxygen-rich conditions.
- Neurological inflammation: Conditions with nerve irritation may benefit from improved cellular energy and reduced inflammatory pressure.
- Chronic pain syndromes: HBOT may help regulate pain processing and calm inflamed soft tissue.
These effects vary by individual. Some people notice improvements in pain or stamina, while others primarily benefit in healing and recovery time during flare periods.
Access to HBOT and the Patient Experience
Many people seek treatment environments that feel steady, supportive, and medically informed. This is one reason individuals explore oxygen therapy Los Angeles as part of their long-term wellness strategy. In areas where modern centers are available, patients often appreciate having a calm setting that allows sessions to feel more restorative. A consistent environment makes it easier to follow multi-session treatment protocols, which is essential for any therapy that works cumulatively.
Patients typically spend the session relaxing, listening to music, or meditating while the chamber reaches therapeutic pressure levels. The gradual pacing helps people tolerate the treatment, even if they are managing fatigue or chronic pain.
How HBOT Differs From Typical Inflammation-Reducing Therapies
Hyperbaric oxygen therapy works differently from medications that suppress inflammation chemically.
- Broader tissue support: Instead of blocking immune activity, HBOT strengthens the environment where healing happens.
- Improved oxygen delivery: Chronic inflammation restricts blood flow, and HBOT helps deliver oxygen deeper into damaged tissue.
- Natural immune modulation: Increased oxygen can calm overactive immune signaling rather than shutting it down abruptly.
- Recovery enhancement: Tissue damaged by a flare or injury may recover faster when oxygen supply improves.
These distinctions explain why HBOT is often used alongside medications, lifestyle changes, and physical therapy. It strengthens biological processes rather than replacing standard treatments.
Subnote: People with long-term inflammation often deal with slowed healing because damaged tissues struggle to take in oxygen. HBOT directly addresses this obstacle.
Safety, Risks, and Important Considerations
HBOT is widely considered safe when administered by trained personnel, but it must still be approached thoughtfully.
- Ear and sinus pressure can occur during pressurization, similar to airplane takeoff.
- Fatigue after sessions is common but temporary.
- Rare complications include oxygen-related irritation or difficulty with pressure equalization.
- Medical evaluation is essential for people with lung issues, severe sinus problems, or unmanaged infections.
Did you know?
HBOT was originally developed for treating decompression sickness in divers, long before it became a tool for inflammation and tissue healing.
A careful medical review ensures that HBOT is used safely and effectively, especially for people managing multiple conditions or long-term medication regimens.
Who Might Benefit Most From HBOT

People with chronic inflammation often fall into patterns of slow recovery, persistent swelling, or fatigue that disrupts daily life. HBOT may be especially helpful for:
- Individuals whose tissue healing is consistently delayed.
- People experiencing joint or soft-tissue inflammation that does not fully respond to medication.
- Patients recovering from surgery or flare-related injury.
- Those with chronic pain syndromes where inflammation and poor oxygen supply interact.
- Anyone seeking a complementary therapy that supports energy production and circulation.
HBOT is most effective when used in a structured plan, not sporadically. Benefits tend to accumulate across sessions, especially when paired with comprehensive care and stable lifestyle habits.
Final Perspective
Autoimmune and inflammatory conditions often place long-term pressure on the body, affecting energy, comfort, and quality of life. Hyperbaric oxygen therapy cannot solve the underlying immune dysfunction, but it may support healing, reduce inflammation, strengthen tissue resilience, and ease symptoms that affect day-to-day functioning.
When combined with medical supervision and a realistic understanding of its role, HBOT can be a meaningful addition to a broader treatment strategy. Many people describe feeling steadier, recovering more efficiently, and navigating flare periods with greater control.









