Are you putting much time into your small practice’s software research? Choosing a solution can take time due to the extensive range of features that providers offer.
Did you know that 40% of medical bills have mistakes on them? Either the healthcare facility or the patient suffers losses due to these mistakes. They also result in more medical claim denials.
With the help of healthcare billing software, offices may run more smoothly, with less paperwork needing to be tracked. Doctors no longer need to waste valuable administrative time searching for documents and retrieving patient records from off-site storage facilities. By preventing claim denials and the potential of sending claims inadvertently formatted, medical billing software can save money.
Regardless of the size of your practice or your prior experience with using medical software, it would be best if you had a firm grasp of the functions of the software to avoid wasting time or money on a new tool. In contrast to practices that outsource their billing, the claims management capability may be applicable to in-house billing practices.
If your healthcare facility has this many mistakes, avoid putting the burden on yourself. Most of these undoubtedly occurred while you were performing your primary responsibility, caring for patients.
Top Features To Be Included in Medicine Billing Software

1. Claims Administration:
Medical billing reporting needs claims management services to save time and reduce errors. Medical billing, coding, and claim processing are organized through a claims management software function. Credentialing applications can be integrated with medical billing software to handle claims for medical billing and coding.
Patients who use medical claims management can quickly determine how much they owe the hospital. Although the process can be carried out manually, it takes a lot of time and has a significant likelihood of error.
To collect, fill out, and process these claims, your team should have assistance from the medical billing system. Before being sent to clients, the program should also assist in validating claims and claim codes.
2. Financial Management:
Software for medical billing that accepts a variety of payment methods is efficient. The revenue cycle system must be adaptable enough to handle patient requests, from cash to credit cards. As the preferred payment method in the future, a revenue cycle management system that takes credit card payments is essential. Flexible payment alternatives significantly improve hospital management, whether at the time of healthcare scheduling or post-care payment. Financial management has the potential to dramatically improve healthcare payment when integrated into the fundamental functions of the integrated healthcare system.
3. Patient Preregistration
This process is an essential part of medical billing information. A precise and reliable method of patient preregistration considerably improves the billing workflow. Patients can enjoy a higher level of satisfaction through shorter wait times thanks to this process, which serves as healthcare management’s onboarding and inflow process. An integrated healthcare model also offers overall efficiency, focusing on patient history, insurance eligibility, and Medicare provider enrollment.
This preregistration approach helps lessen vulnerabilities to billing problems because preliminary data is already acquired during appointment scheduling. An appointment management system of automation in healthcare can combine scheduling software with medical billing components.
4. Eligibility Verification
Less than 25% of physician practices have the necessary checks in place, which shows how frequently eligibility verification is disregarded. However, reliable insurance verification can maintain a sound revenue life cycle.
Patients might need to be fully aware of all the facts affecting their out-of-pocket costs due to the complexity and complication of insurance contracts. Real-time patient eligibility verification includes various information, including demographics, co-pays, deductibles, insurance coverage, and more, to speed up check-ins, lower the likelihood that claims will be denied, and give patients all the facts, so they are not caught off guard by sizable bills.
5. Electronic Remittance
Insurance companies that offer ERA forms give your practice better record-keeping capabilities. A feature of medical billing software lets you import data regarding payments that have already been posted. This enables you to quickly follow payment details for all the claims readily available on your accounts.
6. Automated Accounting
Medical billing and coding analysis utilizing medical document management, medical billing codes, insurance claims management, Medicare and Medicaid coverage, accounts receivables, and the overall healthcare revenue cycle is all included in automated accounting in the medical billing software. The entire billing process is simplified when all of these procedures are automated through interoperability in healthcare. Additionally, fewer claims are rejected or refused thanks to error-free invoice and bill creation.
Automated accounting features, including electronic billing, automated payment reminders, seamless medical billing, and coding, improve revenue cycle management. This can be regarded as a critical element of the billing software used by medical billing organizations.
7. Patient Database
While a central patient database offers benefits of its own, integrated health information systems perform better in medical coding and billing. The advantages are significantly more significant when the medical billing software gets continuous, immediate access to the updated patient database via connected health systems.
To improve the revenue cycle for healthcare, medical billing businesses must ensure that the medical coding and billing department has access to EHR/EMR systems. Finally, it provides access to various information, including medical records, Medicare eligibility, prescription drug coverage, etc.
8. Scheduling
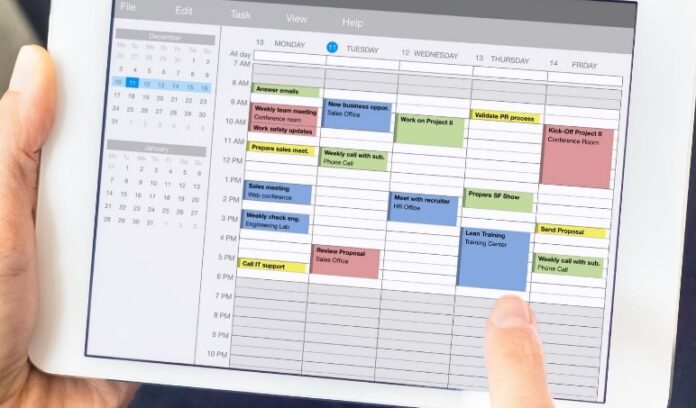
Medical billing services depend on patient appointment scheduling information to verify the correctness of medical billing codes. Medical coding and billing can be significantly streamlined by accessing patient inflow, treatment specifics, appointment types, and revisits. Health systems integrated into the software are more effective because they depend on one another for accuracy. The ideal element of a successful healthcare payment system is an easy-to-use interface that uses a single platform for scheduling and billing.
9. Compliance
Compliance strength is one of the many qualities that should come first in medical billing services. Without compliance included in integrated health information systems, there is a greater likelihood of facing legal action. This might deal with the RCM in healthcare severe damage. Keeping up with changing medical laws manually is challenging. So, maintaining HIPAA compliance standards requires automation inside your software’s compliance component. You can confidently refer to this feature as the software’s core functionality.
10. Automated Reporting
Financial reports, patient records, and claims reporting are regularly needed elements and should be available to deliver effective medical billing services. A good medical billing program should be able to retrieve and update these reports automatically. Robust reporting systems provide seamless billing and care delivery processes, resulting in efficiency. A practical methodology is ideally an intelligent dashboard that connects all patient-related data.
Getting any report from the hospital should be simple for you if you have medical billing software. The hospital administration primarily uses the reporting channel to summarize hospital activity.
11. Encryption and Security
Your medical billing system contains confidential information, especially regarding your patients. Because of this, it is your moral and legal responsibility to ensure this data is well-protected.
First, the Health Insurance Portability Act should be followed by the medical billing systems you utilize (HIPAA). This law safeguards the confidentiality of patient data in healthcare institutions.
Keep in mind that you have private financial and medical information. If uninvited parties discover this date, bad things might happen.
Additionally, this data needs to be protected using encryption both in transit and at rest, especially when kept in cloud memory. In this way, even if someone gains access to the data, they will be unable to retrieve any information. It’s also essential to use secure passwords, particularly those that can only be used once.
When such security measures are in place, your patients are more at ease using your medical facility. Their private information is protected from intruders and from being misplaced or destroyed.
12. Claims Rejection Analysis
If a patient rejects a claim, the billing software should be used to handle the situation.
The software can then generate a report of the claims that were denied, together with an explanation of why. Inaccurate patient information, inaccurate clinical data, and inaccurate insurance information are a few of these causes.
The system should analyze the rejected claim, make the appropriate adjustments, and transmit the proper share. This saves a lot of time your personnel could otherwise spend trying to identify a claim’s inaccuracy.
13. Integration with EHR/EMR

Electronic medical records (EMR) and electronic health records (EHR) are rapidly taking over the healthcare sector. 96% of non-federal hospitals had EHR systems with HHS certification. Therefore, if you already have an EHR/EMR system, your medical billing software must work well with it (or any hospital or practice management system, for that matter).
By integrating these technologies, you can create a comprehensive platform that will act as a single source of truth, closing any information gaps and giving you a constant 360-degree perspective of your patients. This saves time for all of your medical team and boosts productivity in a much-needed way.
Conclusion
As you concentrate on your medical career, it is upsetting to witness the struggle of certain areas in your healthcare institution, such as finances. Fortunately, the development of medical billing systems has made it possible to maintain high-quality healthcare delivery while streamlining all other procedures.
A robust solution must provide excellent assistance by phone, web, and email. Another valuable resource for medical workers to have access to continuously is training documentation. You may be sure that your chosen billing software complies with all of the qualities above, ensuring billing success in the present and the future.